Lots of patients come to me struggling with anxiety and eating disorders and aren’t ready to address the eating disorder, but want their anxiety to get better. Their anxiety is often super distressing, and they want relief from their suffering. On the other hand is the patient’s eating disorder, which they may not want to address or even acknowledge its existence.
Trust me, I want to provide relief for the patient’s anxiety. I understand patients with eating disorders are often greatly suffering from their anxiety symptoms as well. I’m often stuck in a catch 22. Patients want to get treatment for their anxiety, but treat their eating disorder? No way! Here’s the problem: I can’t treat one without treating the other.
Anxiety disorders are what we call ego dystonic, meaning they’re distressing to the individual and the individual recognizes that it’s a problem. However, eating disorders for some patients, can be ego syntonic, meaning they’re not distressing and the individual doesn’t see them as a problem. It’s really difficult to treat people for a disorder they don’t recognize is a problem.
Anxiety disorders are hugely prevalent in patients with eating disorders. About two thirds of people with an eating disorder also have an anxiety disorder. This makes sense to me. People struggling with general anxiety, worry, and obsessional thinking might find these thought patterns eventually start to zero in on eating and exercise behaviors. A patient suffering with both anxiety and an eating disorder are often in a nutritionally deficient state. This is a key difference.
When a person is in a nutritionally deprived state, his or her brain isn’t functioning at full capacity. Dr. Kim McCallum, the founder of McCallum Place Eating Disorder Centers, calls it “hungry brain.” Malnourished individuals experience rigid and perseverative thinking, which are often hallmarks of anxiety disorders. As you can see, symptoms of malnourishment often mimic anxiety symptoms.
We also know that the mainstays of treatment for anxiety (antidepressants) aren’t effective if a person is underweight. Antidepressants work by modulating neurotransmitters. Neurotransmitters are derived from nutrients, and if you don’t have enough nutrients available you can’t make neurotransmitters for the medications to work on. To put it simply, if you don’t have the ingredients (the building blocks for neurotransmitters), you can’t make the recipe for improvement in symptoms (changed levels of neurotransmitters).
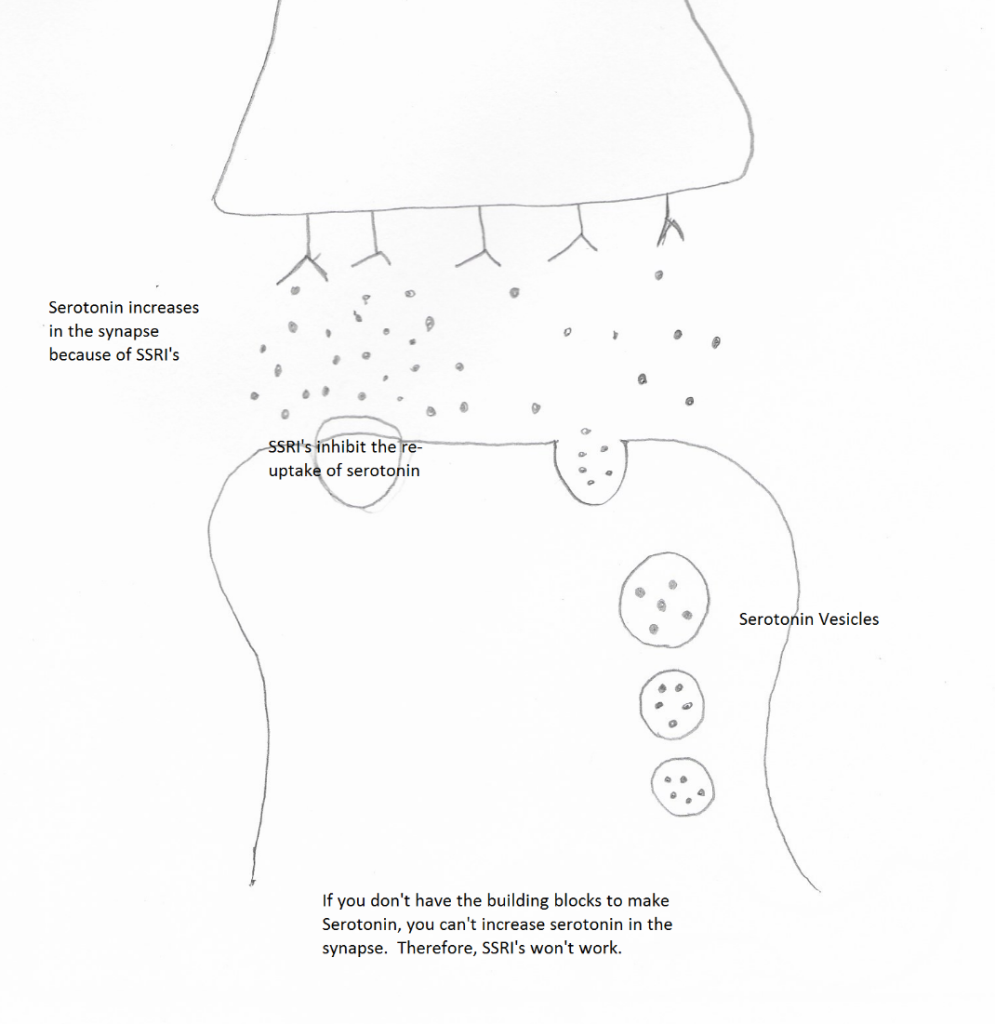
Like my drawing? I was impressed with myself 🙂
So when someone comes to me in a malnourished state wanting help just for their anxiety disorder my response has to be, “I need to help your eating disorder or else your anxiety won’t get better.” It would be impossible for me to make a person’s anxiety better if they’re in a malnourished state. So try to be open to what your mental health care provider recommends when treating your anxiety…and your eating disorder.
References
Kaye WH, Bulik MC, Thornton L, Barbarich N, Masters K. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am J Psychiatry. 2004;161(12):2215–21.
Gregertsen Eva C., Mandy William, Serpell L. The Egosyntonic Nature of Anorexia: An Impediment to Recovery in Anorexia Nervosa Treatment. Frontiers in Psychology. Volume 8, December 2017, Article 2273. URL=https://www.frontiersin.org/article/10.3389/fpsyg.2017.02273
Jimerson DC, Lesem MD, Kaye WH, Brewerton TD. Low Serotonin and Dopamine Metabolite Concentrations in Cerebrospinal Fluid From Bulimic Patients With Frequent Binge Episodes. Arch Gen Psychiatry. 1992;49(2):132–138. doi:10.1001/archpsyc.1992.01820020052007
Josefina Castro-Fornieles, Elena de la Serna, Anna Calvo, Anna Blázquez, Jaime Moya, Luisa Lázaro, Susana Andrés-Perpiñá, María Teresa Plana, Laia Gil, Itziar Flamarique, Esteve Martínez, Jose Pariente, Elena Moreno, Nuria Bargallo, Functional MRI with a set-shifting task in adolescent anorexia nervosa: A cross-sectional and follow-up study, Neuropsychologia, Volume 131, 2019, Pages 1-8, https://doi.org/10.1016/j.neuropsychologia.2019.05.019.
Martine F. Flament, Hany Bissada, Wendy Spettigue, Evidence-based pharmacotherapy of eating disorders, International Journal of Neuropsychopharmacology, Volume 15, Issue 2, March 2012, Pages 189–207, https://doi.org/10.1017/S1461145711000381
Phillipa J. Hay, Angélica M. Claudino, Clinical psychopharmacology of eating disorders: a research update, International Journal of Neuropsychopharmacology, Volume 15, Issue 2, March 2012, Pages 209–222, https://doi-org.beckerproxy.wustl.edu/10.1017/S1461145711000460









